Abstract
Introduction. Limited data exist regarding the role of haploidentical HCT (haplo-HCT) in hemoglobinopathies, whereas long-term outcomes and late effects among these patients are largely unknown. We compared long-term outcomes in two groups of patients underwent halpo-HCT using different in vitro depletion strategies.
Methods. Fifty four consecutive patients, aged <17 years, received a haploidentical (≥2 HLA-mismatched antigens) transplant for thalassemia (n=45) or sickle cell disease-SCD (Hb SS, n=7 and HbS/beta thalassemia, n=2). Among these patients 32 received CD34+ selected PBSC and bone marrow grafts, and 8 patients received CD34+ selected PBSC and CD3+/CD19+ depleted bone marrow grafts between December 2005 and December 2011(group A), whereas 14 patients received TCRαβ+/CD19+ depleted PBSC grafts between June 2012 and March 2017 (group B). The conditioning regimen consisted of oral/weight-based IV BU, Thiotepa (10 mg/kg/d), CY (200 mg/kg) and rabbit ATG preceded by preconditioning with hydroxyurea (30 mg/kg/d), azathioprine (3 mg/kg/d) from D −59, and fludarabine (30-35 mg/m2/d) from D −16 through D −11. Short-course CSA/methylprednisolone or CSA/MMF was given as GVHD prophylaxis until D+60. Eighty and 85% of patients received hematopoietic cells from mother in group A and group B, respectively. The two groups showed similar patient demographics.
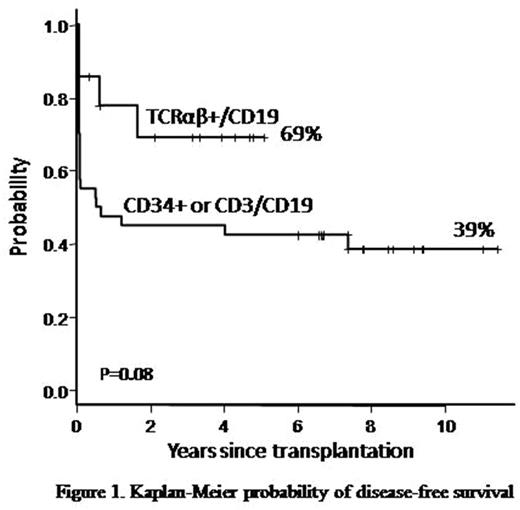
Results. The median follow-up among surviving patients was 90 months (range, 68-139) for group A and 46 months (range, 5-62) for group B. Median CD34+ cell dose in group A and B was 16x106/kg (range, 4.3-28.1) and 15.7 x106/kg (range, 8.1-39.2) (P=0.43), respectively. The grafts of group A patients contained median of 2.8 x105/kg CD3+ and 0.21x106/kg CD19+ cells. The grafts of group B patients contained median of 4x104/kg (range, 1-10.0) αβ T cells, 9x106/kg (range, 2.8-40.2) γδ T cells, 0.06x106/kg (range, 0.01-1.7) CD19+ cells, and 28.67x106/kg (range, 9.8-194.3) CD16+/56+ cells. Sustained engraftment occurred in 55% versus 86% in group A and B (P=0.05), respectively. Group B patients showed significantly faster platelet and neutrophil recovery. Graft failure (GF) occurred in 18 group A (primary GF in 12 and secondary GF in 6 patients) and one patient each in group B had PGF and SGF. The incidence of GF was significantly higher among patients of group A (45%) than of group B (14%) (P= 0.048). Respective OS and DFS were 78% versus 84% (P=0.9), and 39% versus 69% (P=0.085) (Figure 1). The incidence of grade 2-4 aGVHD in groups A and B were 29% and 28%, respectively. Three patients in group A and one in group B developed grade 3-4 acute GVHD with visceral involvement. The remaining patients in both groups had grade 2 acute skin GVHD. The incidence of moderate chronic GVHD was 10% and 21% in group A and B (P= 0.1), respectively. Both groups showed similar CD3+, CD4+, CD8+, CD19+ and CD56+ immune reconstitution with suboptimal CD4+ recovery within the first year: absolute (mean±SEM) cells/ul of CD4+ in group A and B at D+180 were 148±43 and 169±36, respectively (P=0.64). Respective one year absolute cells/ul of CD3+, CD4+, CD8+, CD19+ and CD56+ were 1014±238, 423±97, 559±147, 600±241, 413±151 vs 832±250, 295±74, 415±140, 307±103, 182±49. In group A, 8 patients died due to pneumonia (D+29), perianal abscess (D+33), CMV pneumonia (D+190 ), diffuse large B-cell lymphoma (DLBCL) (D+199), disseminated aspergillosis (D+243), toxic megacolon (+1.2 years), acute heart failure (+ 4 years) and overwhelming postsplenectomy sepsis (+7.4 years). In group B 2 patients died from gastrointestinal bleeding (D+222) or DLBCL (+1.7 years).
The frequency of complications were similar in both groups. The incidence of EBV reactivation/PTLD was significantly higher in patients who did not receive prophylactic rituximab (26%) than who did (4%) (P=0.03).
Conclusions. This study showed that the use of TCRαβ+/CD19+ depleted grafts was associated with a reduced rate of GF and improved DFS compared with CD34+selected/CD3+CD19+- depleted grafts in hemoglobinopathies. However, delayed immune reconstitution and infectious complications remain major causes of morbidity and mortality in these patients. Additional strategies to improve immune recovery are needed.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal